


|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
||||||||||||||
|
|
||||||||||||||
|
||||||||||||||
|
Posted 04/20/2007
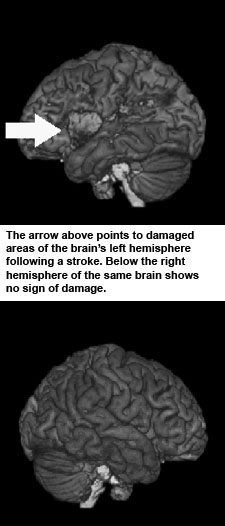
That is something that has nagged Dr. Julius Fridriksson for years. The National Institutes of Health also believes that is a good question and has approved a five-year, $1.62 million grant for the Arnold School of Public Health researcher to seek an answer. “We’ll be looking at potential for recovery, trying to predict who will do well in therapy and who will not,” said Fridriksson, an assistant professor in the Arnold School’s Department of Communication Sciences and Disorders. The study will have a clear impact on public health and important implications for many aging baby boomers and the increasing number of people suffering from obesity, two groups at high risk for stroke. “If you want to research strokes, South Carolina is the place to be. In fact that was one of the main attractions when I came here from the University of Arizona where I got my PhD,” says Fridriksson, Stroke is the third leading cause of death in South Carolina where the disease took 2,631 lives in 2004, according to the S.C. Department of Health and Environmental Control. The state is part of what has been called the "Stroke Belt," a region that generally includes Alabama, Arkansas, Georgia, Louisiana, Mississippi, North Carolina and Tennessee where stroke death rates are substantially higher than the rest of the country. Within the stroke belt, the highest stroke death rates are clustered in the Coastal Plains regions of Georgia and the Carolinas. This region has been called the "Stroke Buckle." Statistics from DHEC indicate strokes disproportionately affect African American men. With a 33 percent higher rate than that of white men, African-American men had the highest stroke mortality rate in all of the race and sex groups in 2004, according to the agency. Fridriksson is putting together a team that will work very closely with a group of 60 volunteer stroke victims over the next five years. Many of them are expected to come from the stroke recovery groups at the USC Speech and Hearing Center where they receive therapy to improve their language function. Others will come from Palmetto Health Richland where the USC Medical School will employ a nurse who will focus exclusively on stroke care and stroke research. The researchers will use a state-of-the-art magnetic resonance imaging (MRI) machine to examine the brain physiology of the volunteers before and after treatment. The purpose is to see if it is possible to predict recovery in stroke victims and to identify those parts of the brain that assume control of functions impaired by the stroke, Fridriksson said. The brain scans will be conducted at the McCausland Center for Brain Imaging at Palmetto Health Richland. In addition to advancing medical knowledge, the study also has a service component. The participants get all of their treatment free and for much longer than Medicare or private insurance is usually willing to pay. Fridriksson says medical insurance hasn’t kept pace with the research when it comes to stroke treatment. “A lot of payment for treatment is offered early on following a stroke when the brain is really not ready for treatment and people just haven’t adjusted. This is the time when insurance companies and Medicare pay the most money,” he said. A better approach would probably be to hold onto the money and pay for treatment later, he said. In fact, studies in animals indicate that intensive treatment very early following a stroke can actually worsen a patient’s condition, he said. |
| Columbia, SC 29208 • 803-777-7000 • sphweb@gwm.sc.edu | © University of South Carolina Board of Trustees |
 Why
do some people recover nearly completely following a stroke while others
remain impaired for the rest of their lives?
Why
do some people recover nearly completely following a stroke while others
remain impaired for the rest of their lives?